Measles Alert:
Are you Protected?
Measles is one of the most contagious diseases that can affect humans. It can be a serious disease for pregnant people. Measles is almost entirely preventable with the measles-mumps-rubella (MMR) vaccine.
From an all-time low in 2000, measles cases have been increasing in recent years. Most reported cases now happen in people who are not vaccinated or didn’t complete their vaccinations as children.
Measles can be a serious disease for pregnant people. Pregnant individuals with measles are more likely to develop measles complications, such as pneumonia. Having measles also increases the risk of pregnancy problems such as preterm birth, low birth weight, infections in the newborn, stillbirth, and miscarriage.
Here’s what you should know about measles and how to protect yourself and your baby.
-
Measles is caused by a virus that is easily spread. The virus can remain in the air for up to 2 hours after an infectious person coughs or sneezes. Just one infected person can cause 14 to 18 additional measles cases.
-
Exposure to measles means being in the same room at the same time or within 2 hours of a person with measles.
-
Measles symptoms can start anywhere from 6 to 21 days after being exposed to the virus, although 11 to 12 days is the average. A person may start spreading the virus to others before they develop symptoms.
Many people have no symptoms or only mild symptoms. When they occur, signs and symptoms may appear in the following order:
Days 1 to 2: Fever, cough, runny nose, and sore eyes can occur. The fever may go very high (spike) to 104 or higher.
Days 3 to 5: A rash begins on the face and spreads downward to the neck, upper and lower trunk, and arms and legs. The fever may spike to 104 or higher.
Days 6 to 7: The rash starts to fade in the order it appeared.
Complications of measles occur in about 3 in 10 people and include ear infections, blindness, pneumonia, and brain inflammation. In the United States, death from measles is rare but can happen. In other countries, it is as high as 15%.
-
Pregnant people with measles have an increased risk of pneumonia, hospitalization, and the need for breathing support. Measles can also increase the risk of pregnancy complications, including miscarriage, stillbirth, low birth weight, and prematurity.
-
You’re protected against measles if you have a written record of one the follow:
You had 2 doses of the measles vaccine as a child
You had one dose of the measles vaccine as an adult
You had measles as a child
You had a blood test that shows you are immune to measles
You were born before 1957
If you do not have a written record of one of the above, you should get 1 dose of the MMR vaccine as an adult.
-
The MMR contains a live, weakened form of the measles virus. Pregnant people should not get the MMR during pregnancy. You can get the MMR vaccine:
Before pregnancy, and wait at least 4 weeks after getting the MMR vaccine to get pregnant
Anytime after you have your baby
Vaccination while breastfeeding is safe. Your family members can be safely vaccinated with MMR; they won’t pass the virus to you.
-
Call your healthcare professional. They will ask if you have a written record of vaccination. If you don’t, you can have a blood test to see if you are immune.
If you have records showing you’re vaccinated, or your blood test results show you’re immune, no other care is needed. You’re protected against measles.
If you are not protected, a medication called immune globulin (IG) can be given within 6 days of being exposed to measles. This medication is given as a shot or through an IV.
If you don’t get measles, you should get the MMR vaccine after you give birth to your baby.
-
There is not a specific cure for measles, so treatment focuses on relieving symptoms and managing complications. Common treatments include:
Rest and fluids to help your body recover
Pain relievers or fever, such as acetaminophen, to reduce fever and discomfort
Antibiotics if you develop a bacterial infection, like pneumonia
Oxygen and other treatments if you experience series complications like trouble breathing
For children with measles, Vitamin A may be used to help improve recovery, but it’s important that it is given in the proper doses. High doses of Vitamin A can be toxic and should only be taken under the guidance of a healthcare provider.
If you are pregnant, Vitamin A treatment for measles is not safe. High doses, above 10,000 units daily, can cause serious birth defects. There is no clear information about how Vitamin A affects breastfeeding, so always talk to your doctor before taking any medication or supplement while breastfeeding.
-
Yes, you can continue breastfeeding if you’ve been exposed to measles or have been diagnosed with measles. However, to help reduce the risk of transmitting the virus to your baby, please follow these precautions:
Wear a facemask when breastfeeding or in close contact with your baby.
Wash your hands thoroughly before each breastfeeding session.
Limit skin-to-skin contact with your baby for up to 3 days to reduce the spread of germs.
Consider using a breast pump to express milk, which can then be given to your baby in a bottle.
Measle Images
A measles rash after 3 days. (CDC/PHL)
Measles rash on a young child. (istock)
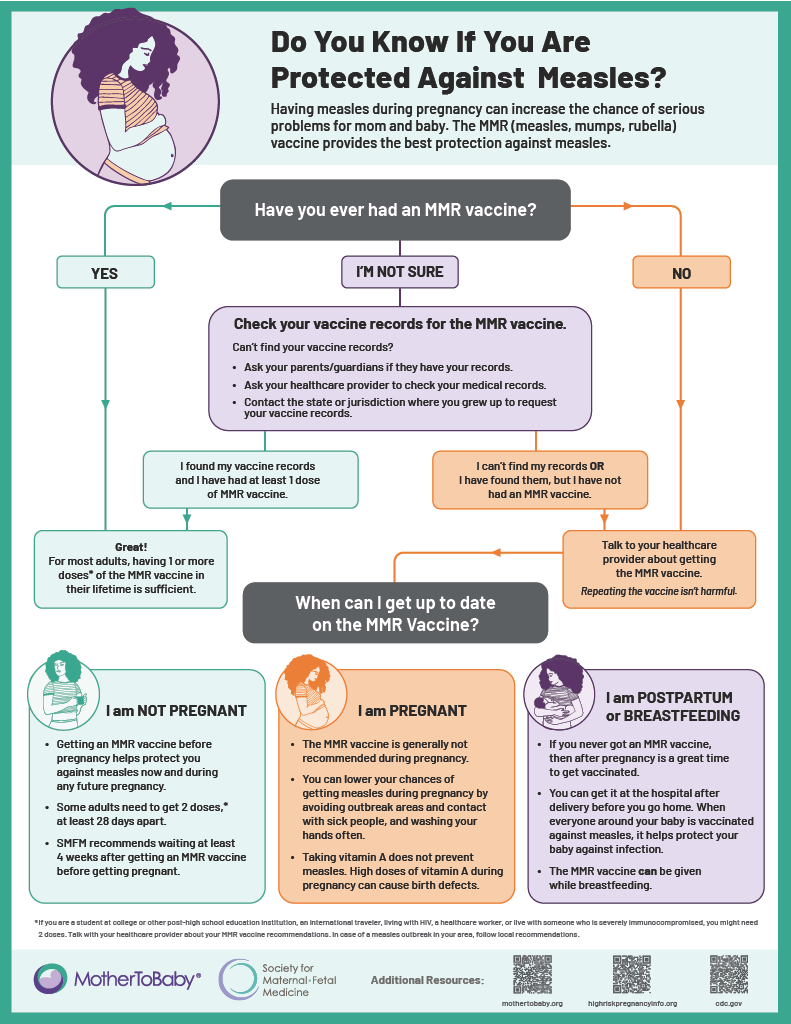
Do You Know If You Are Protected Against Measles?
Getting measles during pregnancy can lead to serious health risks for both you and your baby. The MMR (measles, mumps, rubella) vaccine is the best way to protect yourself.
Not sure if you're protected? Use the flow chart to help you determine your next steps.
Quick Facts
Measles is a highly contagious disease that’s preventable with the measles-mumps-rubella (MMR) vaccine.
Measles can be a serious disease for pregnant people, who are more likely to develop complications like pneumonia. It can cause pregnancy-related problems like preterm birth, low birth weight, infections in the newborn, stillbirth, and miscarriage.
The MMR vaccine is typically administered during childhood. The first dose is given between 12 to 15 months of age and the second between 4 to 6 years of age.
Adults who are unsure of their vaccination status and either don’t have a written record that they were vaccinated or don’t have written proof of immunity should get vaccinated.
Because MMR is a live vaccine, it should not be given during pregnancy. People getting the MMR vaccine should wait at least 4 weeks before trying to get pregnant.
Last Updated: April 2025
This resource was supported by the Society for Maternal-Fetal Medicine (SMFM) and the Centers for Disease Control and Prevention (CDC) cooperative agreement CDC-RFA-DD-23-0004 Enhancing Partnerships to Address Birth Defects, Infant Disorders and Related Conditions, and the Health of Pregnant and Postpartum People. The views expressed by the authors do not necessarily reflect the official policies of the Department of Health and Human Services nor represent an endorsement by the U.S. Government.